Background:
T-cell acute lymphoblastic leukemia/lymphoma (T-ALL/-LL) is an aggressive hematological neoplasm originates from T-cell progenitors. T-ALL and T-LL are distinguished by the presence of more or <20% marrow blasts, respectively. Allogeneic hematopoietic cell transplantation (SCT) is typically recommended for adults with T-ALL in second or later complete remission (CR2+), but also may be offered to patients in first CR (CR1) with high-risk features. Our center reported previously outcomes of allogeneic HCT (allo-SCT) in 53 adolescent and young adults of T-ALL ( Biol Blood Marrow Transplant. 2012;18(12):1897-1904).
Patients and Methods:
We analyzed the outcomes of adults (age >14years) with T-ALL who received allo-SCT at King Faisal Specialist Hospital and Research Center between January 1985 and September 2018. Patients eligible for allo-SCT included HR patients in CR1 and any patient in > CR2 or relapse. Patients in CR1 had one or more of the following HR features: WBC count at presentation > 100,000/mm3, residual disease in bone marrow (BM) at day 14 postinduction, central nervous system (CNS) involvement at diagnosis and the need for more than one induction regimen to achieve CR1.
Full-intensity conditioning regimens were used for all patients. The majority of patients (95.1%) received cyclophosphamide 60 mg/kg once daily i.v. for 2 consecutive days (total dose, 120 mg/kg), followed by 12 Gy of fractionated total body irradiation (TBI) given in 6 fractions. Seven patients (4.9%) received busulfan 16 mg/kg (1 mg/kg per dose orally every 6 hours over 4 consecutive days) and cyclophosphamide 60 mg/kg once daily i.v. for 2 consecutive days (total dose, 120 mg/kg).Short-course methotrexate plus cyclosporine (MTX/CSA) was the GVHD prophylaxis regimen used, in all patients.
Results:
143 patients underwent allo-SCT and were included in this study; some of them were referred in CR for allo- SCT after undergoing induction chemotherapy outside our institution. Median age was 20 years (range, 14-52).Majority of patients were males 116 (80.6%). Extramedullary presentation was reported in 34 patients (23.8 %) with CNS involvement in 15 patients (10.5%).
For SCT outcomes, the incidence rates for relapse 27.1%, acute GVHD 45.8%, grade II-IV acute GVHD was 29.9% and that of chronic GVHD was 38.9%, extensive chronic GVHD was 21.5%. GVHD relapse free survival (GRFS) was reported in 27.1%. The majority of relapses occurred within 1 year after SCT. The cumulative incidence of relapse (CIR) at 1 year was 22.4% 95% CI (15.9 - 29.5), at 2 years was 23.8.8% 95% CI (17.2 - 31) and at 5 years was 25.9% 95% CI (19 - 33.3). Other outcomes, Hemorrhagic cystitis (HC) was noted in 9.7%, sinusoidal obstruction syndrome (SOS) 9%
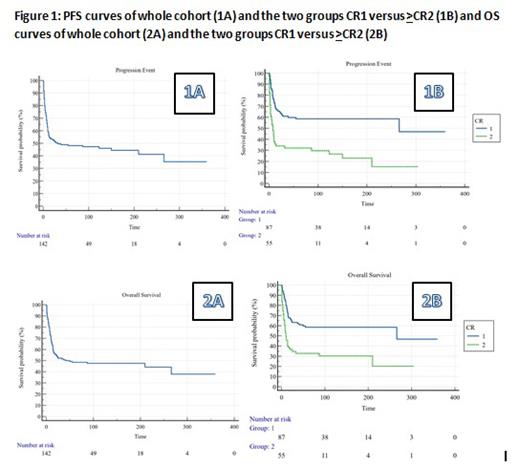
The mean time for overall survival (OS) was 166.77 months (95% CI = 136.54 - 197), and the median survival time was 41 months (95% CI = 15 - 266). For the CR1 group was 205.63 months (95% CI = 166.59 - 244.66). At 10 years, OS of the CR1 group was 74.44 months (95% CI = 63.67 - 85.22), and for the > CR2 group was 35.36 months (95% CI = 24.39 - 46.32); p= 0.0001
PFS analysis showed, the overall mean survival time for disease progression at 5 years was 33.16 months (95% CI = 28.77 - 37.54), and the median survival time was 32 months (95% CI = 12 - 55). For the CR1 group was 39.82 months (95% CI = 34.54 - 45.09), and for the >CR2 group was 22.83 months (95% CI = 16.02 - 29.64), p < 0.0001. At 10 years, PFS for the CR1 group was 74.95 months (95% CI = 63.58 - 86.31), and for the >CR2 group was 41.24 months (95% CI = 27.37 - 55.11) with statistically significantly difference, p < 0.0001.
On multivariate analysis, chronic GVHD was significantly associated with a lower OS (P=0.006) and PFS (P=0.01).Disease status at SCT remained significantly associated with PFS (P=0.02),but not OS (P=0.07). The presence of extramedullary disease and CNS involvement at diagnosis had no effect on the different outcomes.
Conclusions:
Allo-SCT could provide better disease control for HR patients with T-ALL/LL in CR1. Dismal outcomes are reported in patients beyond CR1 with early relapses post allo-SCT are almost inevitable. Better understanding of disease's molecular background in addition to MRD applications, could help to identify more patients in CR1 status who might benefit from allo-SCT. Post SCT strategies including maintenance or pre-emptive interventions might be needed to improve SCT outcomes for T-ALL
Disclosures
Alfayez:Abbvie: Research Funding; Astellas: Honoraria; AstraZeneca: Honoraria; Johnson & Johnson: Consultancy, Honoraria, Research Funding; Amgen: Honoraria; Biologics: Consultancy, Honoraria; Novartis: Honoraria; Pfizer: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal